

2022年更新
(以下文章是母乳喂养医学会临床指南#36《乳腺炎谱系》2022修订版中的信息汇总)
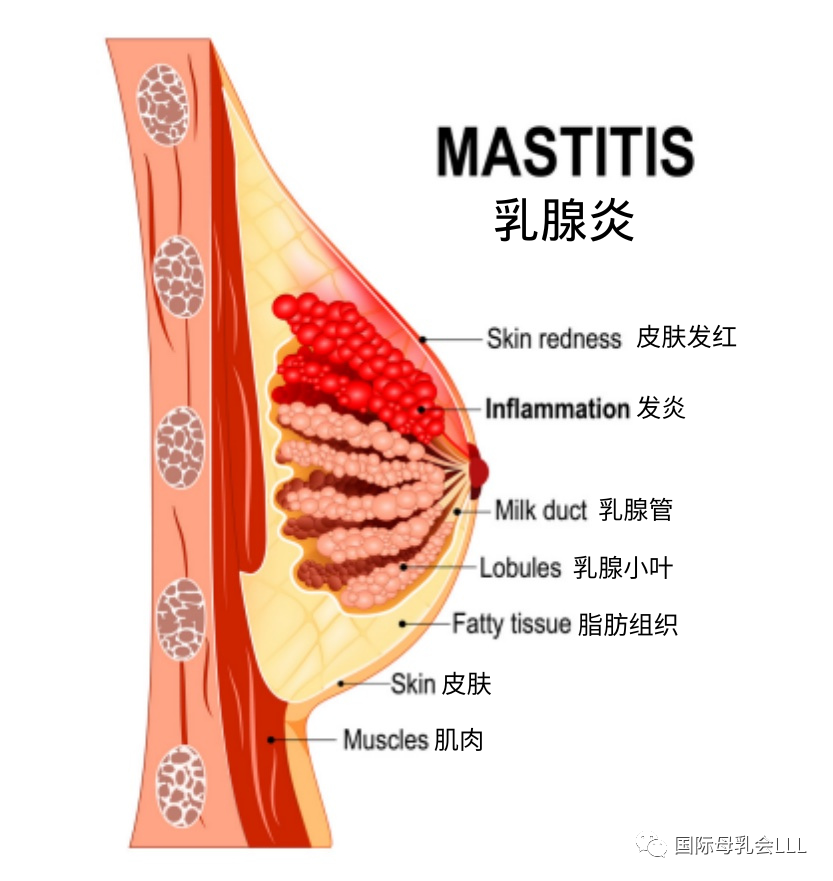
乳腺炎是一系列与乳房炎症相关的症状。您可能从未患过乳腺炎,或者您可能发现自己需要采取些措施来预防其复发。
当您产奶时,在众多输送母乳的小导管(即乳腺管)中,有一些会变得过度充盈。您可能偶尔感到不适或触痛,但婴儿哺乳后或您挤出一些乳汁后就会缓解。
如果您注意到乳房上某个部位发硬、肿胀、发热、疼痛或发红(如果您的肤色较浅),通过哺乳或者吸奶也无法缓解的话,有可能一根或多根乳腺管已经发炎了。
好消息是,护理得当的话,乳腺炎会好转,您能在整个炎症期间一直哺乳。
乳腺炎通常起始于一根乳腺管的单纯炎症,导致导管狭窄,乳汁流动减慢。这通常被称为乳管“堵塞”,实际上并没有一个“塞子”堵在那儿,这个词可能有误导性。
乳腺炎也包括乳腺组织更大面积的炎症。您可能会感到疼痛,伴有发烧、寒战和心动过速,类似于得了流感。有时这种炎症会继续发展为细菌感染,可能需要抗生素治疗。
乳腺炎不会传染。您不需要定期对吸奶器配件、安抚奶嘴或家用物品消毒。尽早治疗可以减轻炎症,有助于避免感染。任何阶段的乳腺炎均可被治愈。
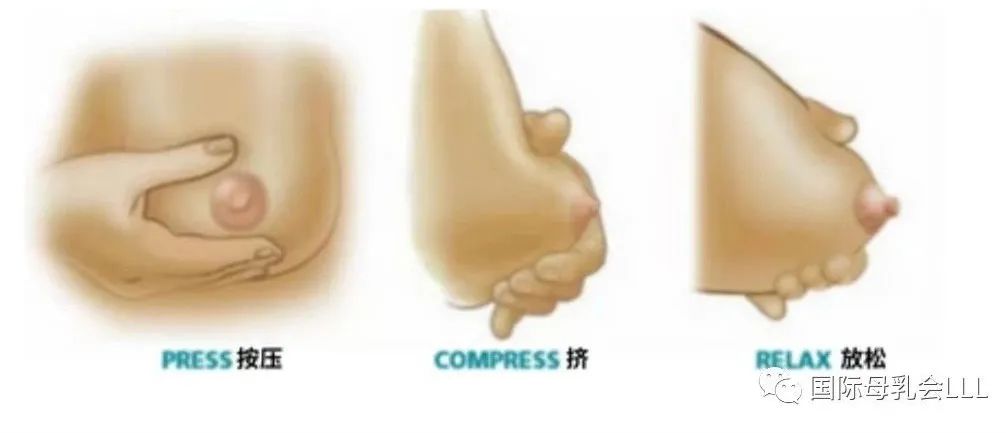
如果您的乳房肿胀,用反向按压软化法同时用手挤出少量乳汁,就可让宝宝更容易地含乳。
如果您的乳房非常疼痛,或您感觉浑身酸痛乏力,可能很难积极地给宝宝哺乳。这时要尽可能多休息,尽量减少生活中的压力,并向国际母乳会中国的哺乳辅导寻求帮助。

图一:乳腺炎早期,发热、发硬、发红、红斑状条纹
图二:症状加重,发热、发硬、发红、水肿。
图三:症状更严重。脓肿形成了一个肿块,正从已红肿的乳腺组织中(图片中上部)突起。



该怎么办?
◆跟随宝宝的喂养信号频繁地哺乳或挤奶,将有助于防止乳房过度充盈。如果您把宝宝时刻放在身边就更容易做到。没有必要“排空”乳房,这会远超宝宝的需求量。
◆将宝宝的下巴对准疼痛部位,可以帮助他更有效地从该处移除乳汁。
◆以下是其他人发现有助于减轻炎症和疼痛的方法:
❶ 每小时敷一次冰/冰袋,如果感觉良好,可以增加频率。
❷ 考虑服用非类固醇抗炎药物如布洛芬来缓解炎症和疼痛。
❸ 必要的话,考虑服用止痛药物,如对乙酰氨基酚。
❹ 考虑服用卵磷脂补充剂(大豆或向日葵),可以减少乳脂的粘性。服用量需遵照包装上的说明。母乳喂养医学会建议每日口服5-10克。 如果您对剂量有疑问,请咨询医护人员。
◆如果您的乳房涨得很不舒服,在喂奶间隙用手挤出少量乳汁可以缓解。请点击“阅读原文”观看手挤奶视频。
◆对乳房深度按摩会加重炎症和组织水肿。您可改为轻轻扫过皮肤并温和地触摸。
☞在您的脖子底部、锁骨上方位置划10个小圈。
☞在您的乳房和腋下交界处划10个小圈。
☞从乳头向胸部、锁骨和腋下轻轻扫过。
◆穿着合身的、支撑好的内衣会更舒服。
◆服用益生菌可能有帮助,它有助于在您体内重建微生物平衡。如果要服用益生菌,里面应含有特定的经证明可有效对抗乳腺炎病原体的菌株。 (请参照下文“乳房怎么了”)。
◆治疗乳头白泡(乳头上的小白点):
❶ 和医护人员讨论是否可在乳头上涂抹外用类固醇乳膏。卵磷脂补充剂可能也有帮助。
❷ 避免在乳头上用盐水浸泡、蓖麻油摩擦和使用其他外用产品。
❸ 不要试着挑开白泡。
使用上述方法后,大多数乳腺炎病症可在数天内消退。如您还需要额外的帮助,请联系国际母乳会的哺乳辅导。
情况没有改善该怎么办?
如果24小时后您仍感觉没有好转,还继续发烧和/或心跳加速(心动过速),请和医生讨论是否要用抗生素。一般不建议使用抗生素,除非怀疑有细菌感染。您可以在用抗生素的同时继续给宝宝哺乳。
治疗性超声(TUS)使用热能来减轻炎症,可能是乳腺炎的有效治疗方法。对几天内尝试了其它方法仍未解决的情况可能尤为有用。专业培训过的理疗师可以提供这项服务。
有时乳腺炎会发展为更严重的情况,称为脓肿,即液体聚集在某个明确的乳房区域并被感染。这种情况下就有必要手术引流。
在抽吸或置管引流后,您可以从患侧乳房继续母乳喂养。如果需要住院,请和医护人员商量能否把宝宝带在您身边,这样就能继续根据婴儿的意愿频繁哺乳了。
如果您反复发作乳腺炎,可让医护人员做乳汁培养来证明是否存在细菌感染和/或识别导致感染的病原体。避免长时间不喂奶或不挤奶也有帮助。
请记住乳腺炎在各个阶段都可治愈。如果您怀疑乳房发炎,请联系国际母乳会的哺乳辅导或医护人员。
乳房怎么了?
就像宝宝的肠道一样,您的乳房也有一个微生物群,它在各种微生物正好平衡时工作最佳。抗生素和过度泌乳(即乳汁过多)都会破坏这种平衡,造成炎症和乳汁微生物群的破坏(称为乳腺菌群失调)。
①抗生素和益生菌的使用
使用抗生素治疗炎性乳腺炎会改变乳房中正常的细菌平衡,实际上增加了进展成细菌性乳腺炎的风险。
抗生素当然可用来治疗细菌性乳腺炎或其它疾病。这种情况下,服用益生菌可能有帮助。
要用的话,里面应含有证明对乳腺炎病原体(即细菌)有效的特定菌株(发酵粘液乳杆菌,以前分类为发酵乳杆菌,或最好是唾液联合乳杆菌,以前分类为唾液乳杆菌)。
②乳汁过多(过度泌乳)
如果您产出的乳汁超出了婴儿的需求,就很可能引起炎症,从而导致乳汁微生物群被破坏(即乳腺菌群失调)。
过度泌乳可能是由于频繁挤出比婴儿所需更多的奶量(例如,为了存奶填满冷冻室),或者是由于常常挤奶至排“空”乳房为止。
乳腺菌群失调本身可造成导管狭窄和炎症,从而进一步破坏乳汁微生物群。
如果您与宝宝母婴分离或纯吸奶喂养,那目标就是只产出宝宝需要的母乳量即可,不需要挤太多。
吸奶器的喇叭罩尺寸合适很重要,这样吸奶才会舒服,乳汁也容易流出。喇叭罩尺寸不合适、吸奶器吸力过高以及吸奶时间过长均会对乳头和乳腺组织造成损伤。
纯吸奶喂养时,婴儿和乳房之间不会互相交换有益微生物。这会增加您患乳腺炎的几率。
通过避免使用吸奶器,以及喂奶间歇觉得乳房胀得难受时用手挤出少量奶,可以调低(减少)奶量。
如果您是纯吸奶喂养,达到挤出宝宝健康生长所需的母乳量即可。
更多信息,请参照国际母乳会中国的母乳喂养信息《如何知道健康、足月的母乳宝宝得到了足够的母乳?》
请点击“阅读原文”观看手挤奶的视频以了解更多信息。
③乳盾
使用乳盾会加重炎症,最好避免使用。它们无法解决母乳喂养问题的根本诱因。如果您很难做到让婴儿含乳含得舒服有效,请联系国际母乳会的哺乳辅导或哺乳顾问寻求帮助。
请记住,母乳喂养可以并且应该在乳腺炎的整个治疗过程中继续进行。如果您需要信息和支持,国际母乳会中国将在此提供帮助。浏览https://www.muruhui.org/?page_id=12616找到您当地的母乳会小组。
如需分享更多关于乳腺炎和治疗方案的信息给医护人员,请参阅: 母乳喂养医学会临床指南#36《乳腺炎谱系》2022修订版。

MASTITIS– A MATTER OFINFLAMMATION
(The following article is a summary of information found in the Academy of Breastfeeding Medicine Clinical Protocol #36: The Mastitis Spectrum, Revised 2022)
Mastitis is the name given to a range of conditions that all involve inflammation in the breast. You may never experience mastitis or you may find that you need to take steps to prevent it from recurring.
As you produce milk, some of the many, many small ducts (tubes) that transport your milk can get overly full. You may occasionally feel discomfort or tenderness that gets better after your baby nurses or you express some milk. If you notice an area that is hard, swollen, warm, painful or red (on lighter skin tones) that isn’t relieved by nursing or pumping, one or more of those ducts may have become inflamed.
The good news is that with supportive care mastitis does get better and you can continue to breastfeed through it all. Mastitis usually starts with a simple inflammation in just one milk duct which causes the duct to narrow, slowing down the flow of milk. This has often been called a“plugged”duct; since there isn’t really a“plug,”this term can be misleading. Mastitis may also involve a much larger area of inflammation in the breast tissue. You may feel achy, with fever, chills and a rapid heartbeat, similar to having the flu. Sometimes this inflammation goes on to become a bacterial infection, which may require antibiotic treatment. Mastitis is not contagious. You don’t need to routinely sterilize pump parts, pacifiers or household items. Early treatment to reduce the inflammation can help you avoid an infection. All stages of mastitis are treatable.
If your breasts are engorged, reverse pressure softening along with hand expression of small amounts of milk will make it easier for your baby to latch.
If your breast is really sore, or you’re feeling achy and rundown, it can be hard to stay motivated about nursing your baby. Get as much rest as possible, do what you can to reduce any stress in your life, and reach out to a La Leche League Canada Leader for support.
What to do ?
◆Nursing or expressing milk regularly, following your baby’s cues, will help prevent the breast getting overly full. This is much easier if you keep your baby close to you. There’s no need to ‘empty’your breasts beyond what your baby wants to drink.
◆Positioning your baby with their chin in line with the sore area can help themremove milk more effectively from that spot.
◆The following are ways others have found helpful to decrease inflammation and pain:
❶ Apply ice/cold packs every hour or more often, if it feels good.
❷ Consider using a nonsteroidal anti-inflammatory drug like ibuprofen to relieve inflammation and pain.
❸ Consider taking lecithin supplements (soy or sunflower) which can reduce the stickiness of milk fat. For how much to take, follow the instructions on the package. The Academy of Breastfeeding Medicine recommends 5- 10 g/day. If you have questions about dosage, consult your healthcare provider.
◆If your breasts are uncomfortably full, hand expressing small volumes of milk between feedings can provide some relief.Click “Read more” to watch Hand Expression Video.
◆Deep massage of your breasts can increase the inflammation and tissue swelling. Instead use light sweeping of your skin and a very gentle touch.
❶ Make 10 small circles at the base of your neck, just above your collarbone.
❷ Make 10 small circles where your breast meets your underarm.
❸ Sweep from your nipple toward your chest,collarbone and underarm.
◆Wearing a well-fitted, supportive bra can be more comfortable.
◆Taking probiotics, which can help reestablish the microbial balance in your body, may be helpful. If probiotics are used, they should contain specific strains shown to be effective against mastitis pathogens (see What’s Happening in the Breast below).
◆To treat a nipple bleb (white bump on your nipple):
❶ Talk to your healthcare provider about applying a topical steroid cream to the nipple. Lecithin supplements can help here too.
❷ Avoid salt water soaks, castor oil rubs, and other topical products on your nipples.
❸ Do not try to open the bleb.
Most cases of mastitis resolve in a few days of using the strategies above. Contact a La Leche League Leader for additional support.

What if things aren′t improving?
If you are not starting to feel better after 24 hours and continue to have a fever and/or fast heart rate (tachycardia),talk with your healthcare provider about the possible use of antibiotics. Antibiotics are not recommended unless a bacterial infection is suspected. You can continue to nurse your baby while you are taking antibiotics.
Therapeutic ultrasound (TUS) uses thermal energy to reduce inflammation and may be an effective treatment for mastitis. This can be particularly useful for cases that do not resolve within a few days of trying other strategies.Trained physiotherapists can provide this service.
Sometimes mastitis progresses to a more serious condition called an abscess. This is where fluid collects in a well-defined area of the breast and becomes infected. In this case, surgical drainage becomes necessary. After aspiration or drain placement, you can continue breastfeeding from the affected breast. If hospital admission is necessary, talk to your healthcare provider about keeping your baby with you, so you can continue to breastfeed as often as your baby likes.
If you have recurring bouts of mastitis, ask your healthc are provider about culturing your milk to verify that there is a bacterial infection and/or to identify the pathogens responsible for the infection. It is also helpful to avoid long periods without feeding or expressing milk.
Remember that mastitis is treatable at all stages. Contact a La Leche League Leader or your healthcare provider if you suspect inflammation in your breast.
What′s happening in the breast?
Just like your baby’s gut, your breasts have a microbiome that works best with the right balance of microorganisms. Antibiotics and hyperlactation (too much milk) can disrupt that balance, resulting in inflammation and disruption of the milk microbiome (called mammary dysbiosis).
Use of Antibiotics and Probiotics
Treating inflammatory mastitis with antibiotics can change the normal bacterial balance in the breast and actually increase the risk of developing bacterial mastitis.
Of course, antibiotics may be needed to treat bacterial mastitis or may be prescribed for other reasons. When that’s the case, it may be helpful to take probiotics as well. If probiotics are used, they should contain specific strains shown to be effective against mastitis pathogens (‘germs’) (Limosilactobacillus fermentum, formerly classified as Lactobacillus fermentum, or, preferably, Ligilactobacillus salivarius formerly classified as Lactobacillus salivarius).
Too Much Milk (Hyperlactation)
If you produce more milk than your baby needs, you are more likely to experience the inflammation that can lead to disruption of the milk microbiome (mammary dysbiosis). Hyperlactation can be caused by frequently pumping more milk than a baby is taking (to build up a freezer stash, for example), or by regularly pumping until the breasts are“empty”. Mammary dysbiosis itself can lead to narrowing of the milk ducts and inflammation, which can lead to further disruption of the milk microbiome. If you are separated from your baby or are exclusively pumping, aim to produce only the amount of milk your baby needs and not more.
It’s important that pump flanges fit well, so pumping is comfortable and milk flows easily. Flanges that are the wrong size, suction that is too high, and pumping for too long can all cause damage to the nipple and breast tissue.
When exclusively pumping, the exchange of beneficial microorganisms between baby and breast doesn’t happen. This may increase your chances of developing mastitis.
Milk production can be downregulated (reduced) by avoiding pump use, and hand expressing small volumes of milk between feedings when your breasts feel uncomfortably full. If you are exclusively pumping, aim to pump only as much milk as your baby needs to grow well.
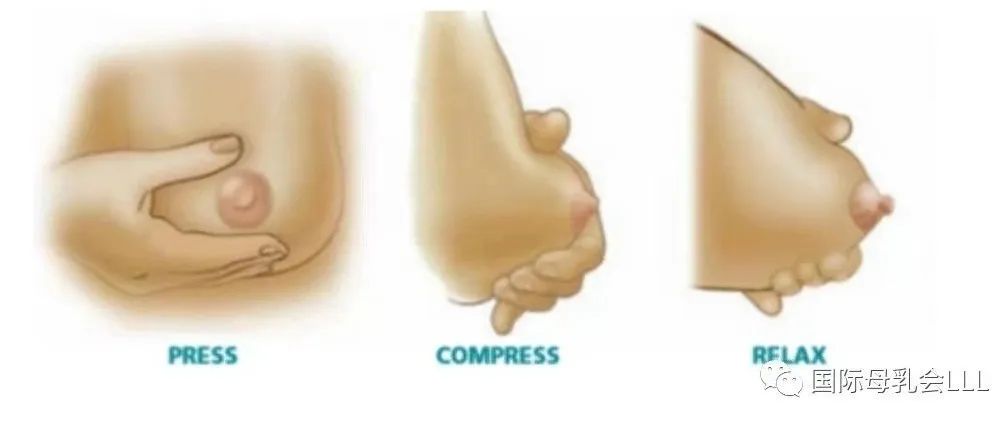
Please Click “Read more” to watch this video to learn more about Hand Expression.
Nipple Shields
Using nipple shields may increase inflammation. It’s best to avoid them. They do not address the underlying causes of breastfeeding problems. If you are having trouble latching your baby comfortably and effectively, contact a La Leche League Leader or lactation consultant for support.
Remember that breastfeeding can and should carry on throughout treatment for mastitis. If you need information and support, La Leche League China is here to help. Click https://www.muruhui.org/?page_id=12616 to find your local LLL Group.
For more information about mastitis and treatment options to share with your healthcare provider, see: Academy of Breastfeeding Medicine Clinical Protocol #36: The Mastitis Spectrum, Revised 2022.

END
翻译:加拿大母乳会,何圆圆
审阅:温传艳,Victoria
编辑:幸宝、沐凡

中国移动手机和宽带用户可访问:
muruhui.com 或muruhui.cn
获取更多资讯
本篇文章来源于微信公众号: 国际母乳会LLL
